Caitlin Notley, Professor in Addiction Sciences, University of East Anglia, UK, in her lecture analysed “Why the UK has taken a compassionate approach to vaping”. She presented the UK approach to smoking control and the consequences of social and cultural influences on behavioural and health long term outcomes; also, she answered to the question whether the approach is indeed compassionate and referred to the remaining challenges. The lecture chaired Dr Dimitri Richter.
Prof. Notley cited the definition on THR according to the Royal College of Physicians, that “harm reduction is a strategy used in medicine and social policy to minimise harm to individuals and/or wider society from hazardous behaviours or practices that cannot be completely avoided or prevented” and commented that this strategy is additional and complementary to tobacco control measures.
Tobacco harm reduction strategy in the UK
Harm reduction approach is pragmatic, stated Prof. Notley. The UK approach is in line with what people are choosing to do, i.e., individuals who smoke who are trying to quit may choose to use different methods: in the general population, most people choose an e-cigarette, which is now a more popular cessation method than nicotine replacement treatment (NRT), as recent UK survey data shows.
E-cigs introduced by Prof. Fagerstrom in 2015, are a consumer product, a disruptive technology, Prof Notley said, which proved to be extremely popular to people as aids to quitting smoking because they mimic both conventional cigarette’s quick nicotine delivery, and behavioural actions of tobacco smoking. E-cigs are mainly used by people who already were smokers and are trying to quit, while most young people don’t take up on e-cigs unless they were smokers, she noted.
The UK approach is also based on evidence of what is effective for smoking cessation, the speaker added, showed a series of recent studies, the most recent being a Cochrane Review published in September 2021 about Nicotine e-cigarette vs NRT, clearly showing that e-cigs were more supportive to people who want to quit smoking; also, Public Health England evidence reviews show vaping to be 95% less harmful than tobacco smoking. Based on the evidence, noted Prof. Notley, a consensus has been reached now across scientific bodies in the UK, that vaping has an important role in tobacco control. No one suggests that vaping is safe, she emphasised, but that in comparison to tobacco smoking, vaping is considerably less harmful to health. Other potential choices are available in the UK as harm reduction practices, such as heat-not-burn products, snus or chewing tobacco, although being much less common.
In terms of communication, NHS campaigns and messages to the public are focusing on switching from cigarette smoking to vaping. Also, guidance is provided to health professionals to assist patients.
Smoking & vaping trends reported in the UK show the important role of vaping in tobacco control, as smoking shows a clear decline. There are also other measures that may have had an impact on smoking rates in the UK, such as smoking prohibition in public places, packaging, hidden points of sales.
The tradition of harm reduction in the UK – How they got here
Professor Notley then summarised how the tradition of harm reduction got where it is today within the British system. She explained that the UK approach has emerged form a specific culture and context. An important element is the strong youth culture in Britain, linked to music scenes and the substance misuse associated with each music culture. Harm reduction has been used to combat substance use, she said, and make youth culture safer (less harmful, yet not risk free).
Cigarette can be described as “iconic” in British youth culture, as cigarettes hold cultural capital in terms of social exchange. They are associated with a social identity, a social group, Prof. Notley said. Today, with e-cigarette we have the potential to replace cigarette with a different equally symbolic icon, but less harmful to health, she concluded.
As to how we got here, specifically as to harm reduction―Prof. Notley continued―harm reduction in tobacco control has not been conclusive in the past. Many things were tried to make cigarettes first less harmful (including lowering tar, lower nicotine, adding a filter). She then referred to the contribution of Professor Mike Russel to tobacco harm reduction concept. He was the first to suggest a shift to less harmful nicotine delivery devices. This was a great paradigm shift in UK harm reduction culture, the speaker said, given that until then abstinence was the end goal. Substitution of nicotine suggested that dependence from nicotine could be acceptable for the population – which also raises a moral issue, one that remains a divide in public health, Prof. Notley said.
The concept of “nicotine addiction” has been medicalised and eventually accepted, the speaker said, and now is part of treatment strategies in the UK. Also, Royal College of Physicians moved away from abstinence to harm reduction. So, today, there is a consensus among stakeholders in the UK that the main tobacco control goal is to reduce the death and disease caused by tobacco use and there is less concern to reduce addiction to nicotine and about eliminating the tobacco industry.
Can the UK approach be considered compassionate?
Concluding, Prof Notley, posed the main question of her talk, whether the UK approach can be considered compassionate or not. On one hand, this approach allows those with nicotine addiction to continue to use nicotine in less harmful ways; there is choice in cessation methods to users. The UK approach may have reduced the stigma of addiction and allowing harm reduction strategies may have levelled up some health inequalities. However, she added, strategies are not uniformly taken up across the social divide, meaning that the UK has still a long way to go before the approach can be considered truly compassionate. On the other side of the compassionate approach, most deprived populations are the most likely to use nicotine in the most harmful way through tobacco smoking; tobacco control measures have further stigmatised entrenched smokers; even vaping may be also stigmatised for some subpopulations.
Remaining challenges
One key remaining challenge is reaching those groups of people who continue to smoke tobacco the most, such as those diagnosed with a serious mental health condition (45% are regular smokers). More needs to be done, the speaker emphasised.
A major challenge set by the UK government is the target to reduce tobacco smoking prevalence of 5% or less by 2030. Looking at the current rates, Prof. Notley pointed out, the UK is not on target to reach this aim.
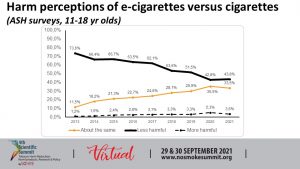
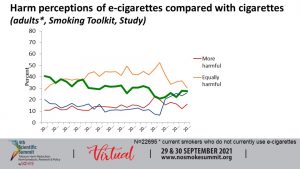
Another challenge is public’s (mis)perceptions of harm that need to be tackled. Around a third of young people think that e cigarettes are as harmful as smoking tobacco, while adults also have inaccurate perceptions.
Finally, divides in the field of THR that question the evidence are unhelpful and feed uncertainty to the public about whether e-cigarettes are a safer option than smoking.
The speaker concluded that in the UK there is a tradition of harm reduction which stems from their cultural and historical approach to harm reduction across substance abuse and other behaviours; an approach that has been shown to have an extremely positive impact on tobacco smoking rates. We might say that the UK approach is compassionate, Prof. Notley said, there is choice & focus on reducing harm not abstinence from nicotine, but key challenges remain: the need to reduce inequalities, to tackle misperceptions about harm reduction and e-cigarettes, and to work in overcoming resistance.